Inferior myocardial infarction (MI) accounts for 40-50% of all MIs. It generally has a more favourable prognosis than anterior myocardial infarction (in-hospital mortality only 2-9%), however certain associated features indicate a worse outcome
ECG diagnostic criteria
- ST elevation in leads II, III, aVF
- Hyperacute T waves may precede these changes
- Reciprocal ST depression in aVL
- Progressive development of Q waves in II, III, aVF
Associated features, all of which confer a worse prognosis, include:
- Concomitant right ventricular infarction (40% of patients); these patients may develop severe hypotension in response to nitrates
- Significant bradycardia due to second or third-degree AV block (20%)
- Posterior infarction due to extension of infarct area
Don’t neglect aVL
- aVL is the only lead truly reciprocal to the inferior wall, as it is the only lead facing the superior part of the ventricle. It is thus a sensitive marker for inferior infarction
- In patient cohorts with inferior occlusion myocardial infarction (OMI), ST depression in aVL has been shown to be more prevalent than STE in inferior leads
- 91% of “subtle” inferior STEMIs that do not meet STEMI criteria but show occlusion on PCI demonstrate ST depression in aVL
Which Artery is the Culprit?
Inferior STEMI can result from occlusion of any of the three main coronary arteries:
- Dominant right coronary artery (RCA) in 80% of cases
- Dominant left circumflex artery (LCx) in 18%
- Occasionally, a “type III” or “wraparound” left anterior descending artery (LAD), producing the unusual pattern of concomitant inferior and anterior ST elevation.
While both RCA and LCx occlusion may cause infarction of the inferior wall, the precise area of infarction and thus ECG pattern in each case is slightly different:
- The RCA territory covers the medial part of the inferior wall, including the inferior septum. The injury current in RCA occlusion is directed inferiorly and rightward, producing ST elevation in lead III > lead II (as lead III is more rightward facing)
- The LCx territory covers the lateral part of the inferior wall and the left posterobasal area. The injury current in LCx occlusion is directed inferiorly and leftward, producing ST elevation in the lateral leads I and V5-6
These differences allow for electrocardiographic differentiation between RCA and LCx occlusion.
RCA occlusion is suggested by:
- ST elevation in lead III > lead II
- Presence of reciprocal ST depression in lead I
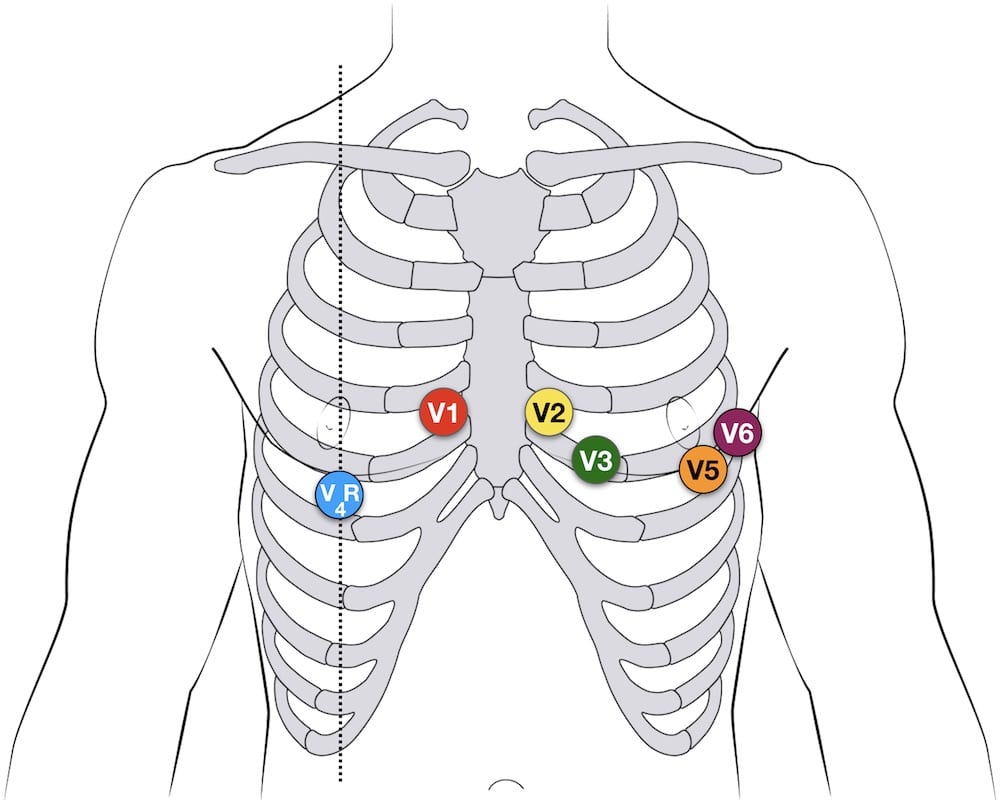
- Signs of right ventricular infarction: STE in V1 and V4R
Circumflex occlusion is suggested by:
- ST elevation in lead II = lead III
- Absence of reciprocal ST depression in lead I
- Signs of lateral infarction: ST elevation in the lateral leads I and aVL or V5-6
ECG Examples
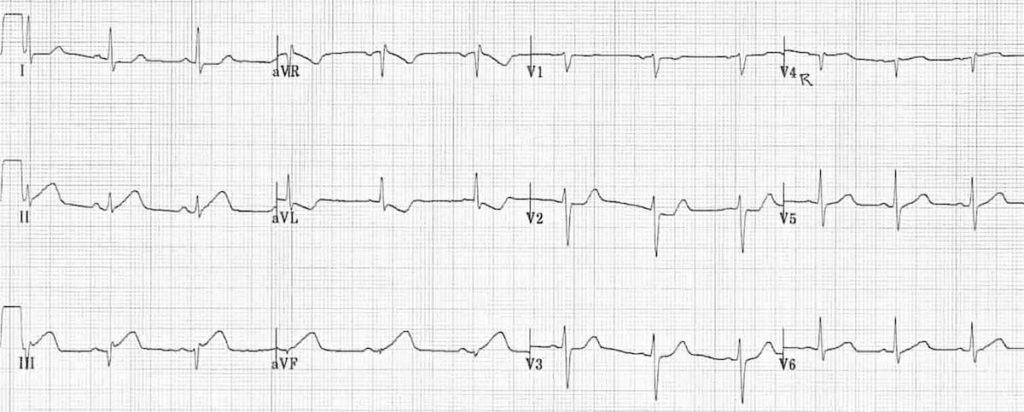
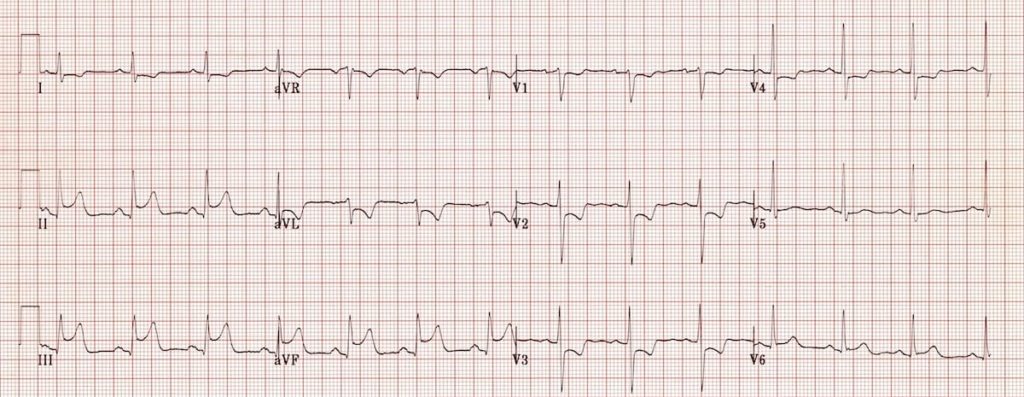
Example 1
Early inferior STEMI:
- Hyperacute (peaked) T waves in II, III and aVF with relative loss of R wave height
- Early ST elevation and Q-wave formation in lead III
- Reciprocal ST depression and T wave inversion in aVL
- ST elevation in lead III > lead II suggests an RCA occlusion; the subtle ST elevation in V4R would be consistent with this.
Note how the ST segment morphology in aVL is an exact mirror image of lead III. The concept of reciprocal change can be further highlighted by taking lead aVL and inverting it. Notice how the ST morphology now looks identical to lead III:
(For more about lead aVL and its utility in diagnosing subtle inferior STEMI, check out this post from Dr Smith’s ECG Blog)
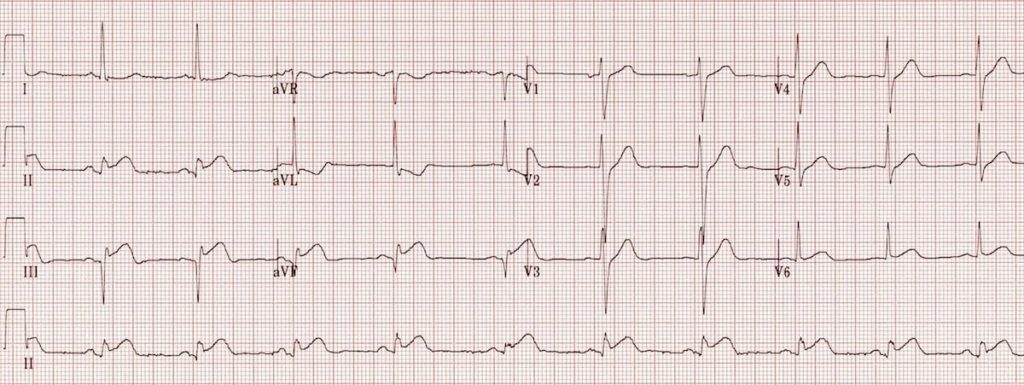
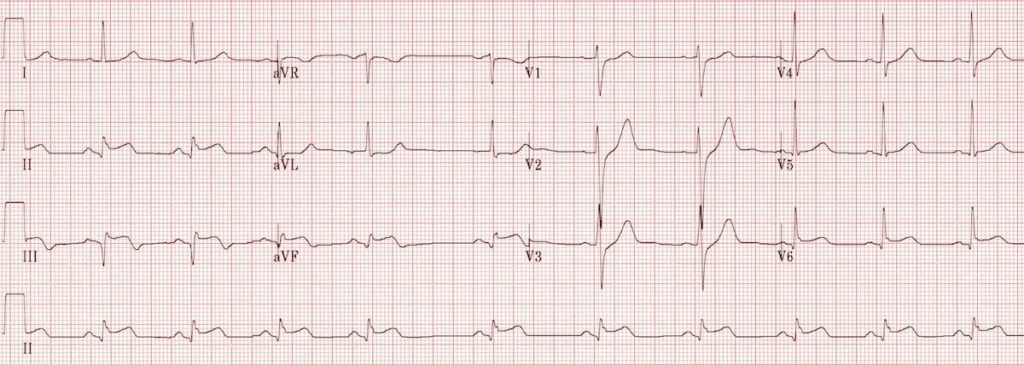
Example 2
Inferior STEMI:
- ST elevation in II, III and aVF.
- Q-wave formation in III and aVF.
- Reciprocal ST depression and T wave inversion in aVL
- ST elevation in lead II = lead III and absent reciprocal change in lead I (isoelectric ST segment) suggests a left circumflex artery occlusion
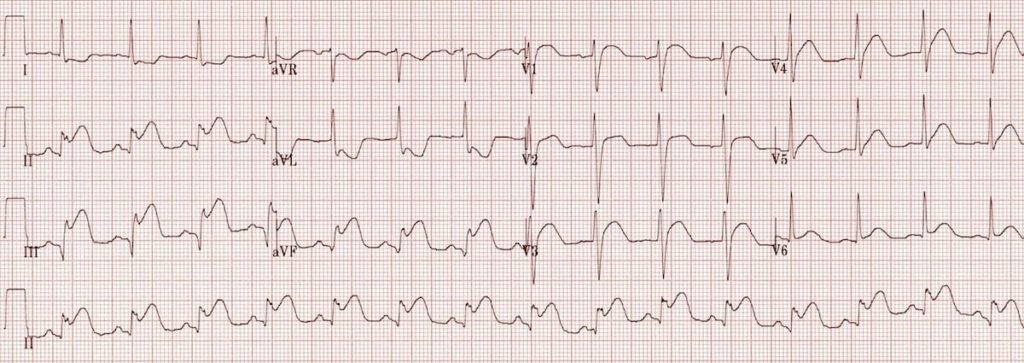
Example 3
Inferior STEMI:
- Marked ST elevation in II, III and aVF with early Q-wave formation.
- Reciprocal changes in aVL.
- ST elevation in lead III > II with reciprocal change present in lead I and ST elevation in V1-2 suggests RCA occlusion with associated RV infarction: This patient should have right-sided leads to confirm this.
Example 4
Hyperacute inferior STEMI:
- Hyperacute T waves in II, III and aVF.
- Early ST elevation and loss of R wave height in II, III and aVF.
- Reciprocal change in aVL and lead I.
Example 5
Inferior STEMI:
- The concave ST elevation in II, III and aVF may be mistaken for pericarditis.
- However, the fact that the ST elevation is localised to the inferior leads with reciprocal changes in aVL confirms that this is an inferior STEMI.
Example 6
Massive inferolateral STEMI:
- Marked ST elevation in II, III and aVF with a “tombstone” morphology
- Reciprocal change in aVL
- ST elevation is also present in the lateral leads V5-6, indicating an extensive infarct of the inferior and lateral walls
In patients with inferior STEMI, ST elevation of 2mm or more in leads V5 and V6 is predictive of extensive coronary artery disease and a large area of infarction.
Example 7
Recent inferolateral STEMI:
- Well-formed Q waves in III and aVF suggest that this STEMI is not acute
- The T waves in III and aVF are beginning to invert
- There is still some residual ST elevation in the inferior (II, III, avF) and lateral (V5-6) leads. ST elevation may take 2 weeks to resolve after an acute inferior MI (even longer for an anterior STEMI)
NB. If this patient had ongoing chest pain you would still treat them as an acute STEMI!
Bradycardia and AV Block in inferior STEMI
Up to 20% of patients with inferior STEMI will develop either second- or third-degree AV block. There are two presumed mechanisms for this:
- Ischaemia of the AV node due to impaired blood flow via the AV nodal artery. This artery arises from the RCA 80% of the time, hence its involvement in inferior STEMI due to RCA occlusion.
- Bezold-Jarisch reflex = increased vagal tone secondary to ischaemia.
The conduction block may develop either as a step-wise progression from 1st degree heart block via Wenckebach to complete heart block (in 50% of cases) or as abrupt onset of second or third-degree heart block (in the remaining 50%).
Patients may also manifest signs of sinus node dysfunction, such as sinus bradycardia, sinus pauses, sinoatrial exit block and sinus arrest. Similarly to AV node dysfunction, this may result from increased vagal tone or ischaemia of the SA node (the SA nodal artery is supplied by the RCA in 60% of people).
Bradyarrhythmias and AV block in the context of inferior STEMI are usually transient (lasting hours to days), respond well to atropine and do not require permanent pacing.
Example 8
- Inferior STEMI with third degree heart block and slow junctional escape rhythm.
Example 9
- Inferior STEMI with sinus node dysfunction (either sinus arrest or extreme sinus bradycardia) and a slow junctional escape rhythm.





No comments:
Post a Comment