Saturday, 27 August 2022
ACS
Friday, 26 August 2022
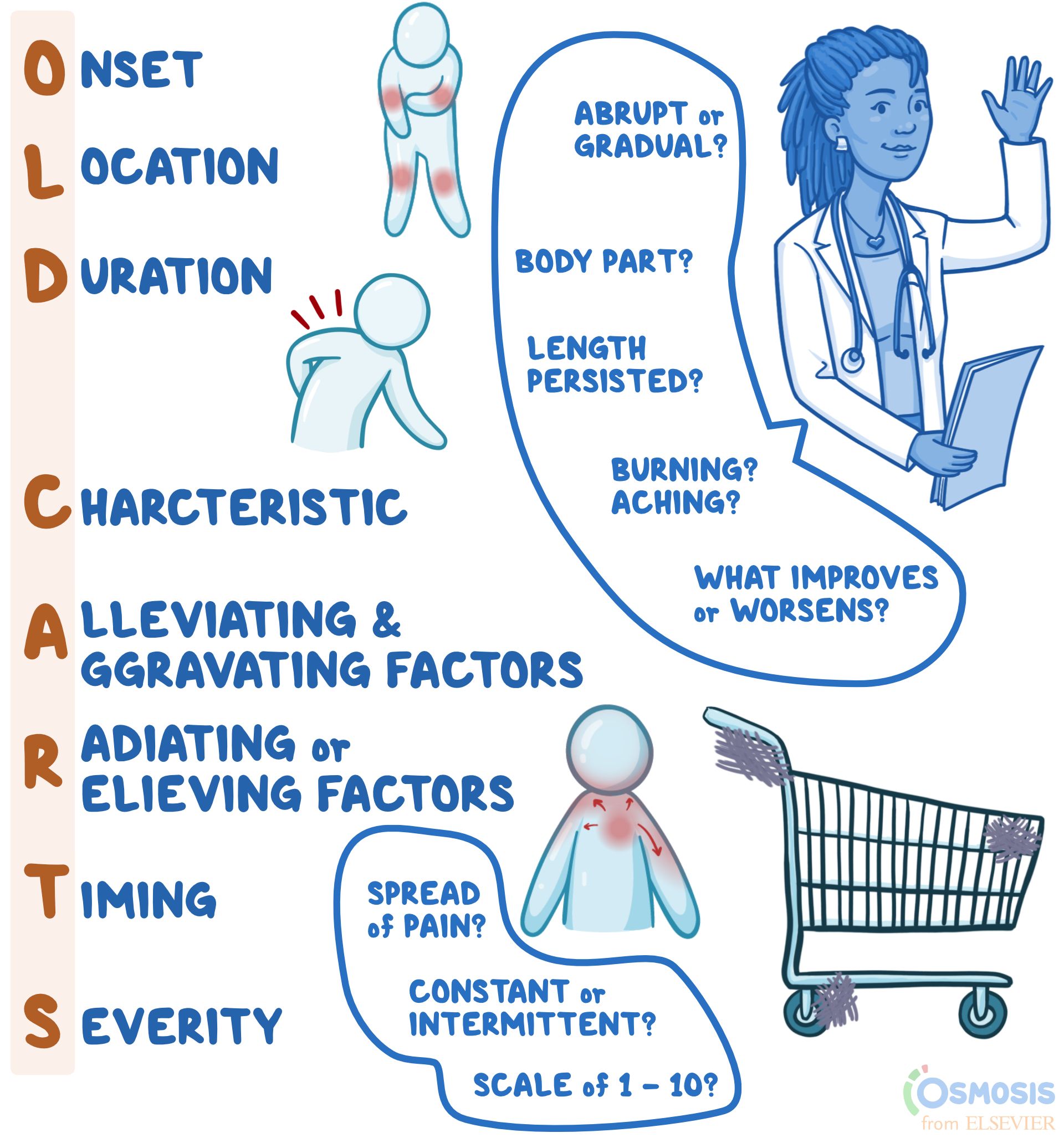
old carts
OLD CARTS
History-taking Mnemonic
Author: Lily Guo
Editors: Alyssa Haag, Ian Mannarino, MBA, MD, Kelsey LaFayette, DNP, RN
Illustrator: Jessica Reynolds, MS
Copyeditor: Sadia Zaman, MBBS, BSc
What does “OLD CARTS” mean?
"OLD CARTS" is a mnemonic device that assists clinicians in remembering the pertinent questions to ask while assessing an individual’s present illness. When a person presents to their clinician with complaints of a new or reoccurring medical problem, the clinician may use "OLD CARTS" as a structured guideline and framework from which they will ask questions and collect information before they perform a physical exam. Most commonly, "OLD CARTS" can be utilized for a patient who is experiencing pain, however, this mnemonic can be used as a framework for any presenting symptom.
What is a history of present illness?
A history of present illness, abbreviated HPI, refers to the description of an individual’s current health complaint, typically described in chronological order from the onset of their first sign and symptom to the present, defined as the moment they are sitting in front of the clinician. It is a narrative written in full-sentence format by the clinician that provides the necessary information for the clinician to generate differential diagnoses, guide medical-decision making, investigate the problem, and ultimately, provide the proper treatment.

Join millions of students and clinicians who learn by Osmosis!
What does the “O” in “OLD CARTS” mean?
The O in OLD CARTS means onset, indicating when and how the complaint began. For example, the clinician may ask if the pain has been present for hours, days, months, or years as well as if the pain occurs abruptly or gradually.
What does the “L” in “OLD CARTS” mean?
The “L” in “OLD CARTS” means location. This refers to where the pain is, including which specific body part (e.g., head, arm, leg, abdomen) and if the pain is isolated to one specific area (e.g., headache isolated to one side of the head, or abdominal pain of the right lower quadrant).
What does the “D” in “OLD CARTS” mean?
The “D” in “OLD CARTS” means duration. This refers to how long or how often the complaint occurs. For example, the pain may last for minutes, hours, or days at a time.
What does the “C” in “OLD CARTS” mean?
The “C” in “OLD CARTS” means characteristic. The clinician may ask the individual to describe their pain using words such as achy, dull, stabbing, sharp, throbbing, squeezing, itching, or burning.
What does the “A” in “OLD CARTS” mean?
The “A” in “OLD CARTS” means alleviating and aggravating factors. The individual may be asked if they did anything to help alleviate the pain, such as taking medications or resting. If they did try home remedies, it would be helpful to know if they improved the symptom. The clinician may also ask if anything worsens the pain, such as changing body position, walking up stairs, or eating.
What does the “R” in “OLD CARTS” mean?
The “R” in “OLD CARTS” means radiation, which refers to whether the pain travels to other parts of the body or whether it is isolated to one region only. “R” in “OLD CARTS” may also refer to relieving factors, or activities or treatments that reduce the pain. The mnemonic may vary slightly depending on the source.
What does the “T” in “OLD CARTS” mean?
The “T” in “OLD CARTS” means timing. This refers to if the pain is constant and experienced at all times, or if it is intermittent, meaning it comes and goes. If the pain is constant, the clinician might ask if the severity fluctuates throughout the day, which is referred to as waxing and waning pain. Meanwhile, if the symptom is intermittent in frequency, clinicians might ask how many times a week, month, or year it occurs.
What does the “S” in “OLD CARTS” mean?
The “S” in “OLD CARTS” means severity. For pain specifically, people are typically asked to rank their level of pain from one to ten, with ten being described as the worst pain they have ever experienced. Other questions to help gauge severity can include asking how the complaint interferes with day-to-day life or how bothersome the complaint is to the individual.
What are the most important facts to know about the “OLD CARTS” mnemonic?
“OLD CARTS” is a mnemonic device used by providers to guide their interview of a patient while documenting a history of present illness. The letters stand for onset; location; duration; characteristic; alleviating and aggravating factors; radiation or relieving factors; timing; and severity. What each letter stands for may vary slightly depending on the source of the mnemonic. Onset refers to when the symptom, for example pain, first began and whether it was abrupt or gradual; location refers to the body part(s) affected; duration refers to the length of time the symptoms have persisted; and characteristic refers to the individual’s description of the symptoms (i.e., burning, aching, sharp). Alleviating and aggravating factors are factors that improve or worsen symptoms, respectively; radiation refers to whether there is any spread of pain; timing refers to whether the pain is constant or intermittent; and lastly, severity is typically ranked on a scale of one to ten, with ten being the most severe. When used to guide documentation of an HPI, the mnemonic “OLD CARTS” can make patient evaluation and management more concise and efficient.
Wednesday, 24 August 2022
Physical health assessment
Physical Health Assessment: Methods and Steps (theworldbook.org)
The Four Methods of Health Assessment
The four basic methods or techniques for physical health assessment are:
- Inspection,
- Palpation,
- Percussion and
- Auscultation.
3 Steps of Health Assessment
- A complete medical history,
- A general survey and
- A complete physical assessment.
1. A Complete Medical History
History taking is the first step of Physical Health Assessment. The general framework for history taking is as follows:
- Presenting complaint.
- History of presenting complaint, including investigations, treatment, and referrals already arranged and provided.
- Past medical history: significant past diseases or illnesses, surgery, including complications, trauma.
- Drug history: now and past, prescribed and over-the-counter, allergies.
- Family history: especially parents, siblings, and children.
- Social history: smoking, alcohol, drugs, accommodation and living arrangements, marital status, baseline functioning, occupation, pets, and hobbies.
- Systems review: cardiovascular system, respiratory system, gastrointestinal system, nervous system, musculoskeletal system, genitourinary system
2. A General Survey
After collecting the health history and before going through the complete head to toe examination, some information or baseline data is collected which is called a general survey.
The general survey includes the person’s weight, height, body build, posture, gait, obvious signs of distress, level of hygiene and grooming, skin integrity, vital signs, oxygen saturation, and the person’s actual age compared and contrasted to the age that the person actually appears like.
For example, does the person appear to be older than his actual age? Does the person appear to be younger than his actual age?
3. A Complete Physical Assessment
A thorough physical assessment consists of the following:
- Vital Signs: The pulse, blood pressure, body temperature, and respiratory rate are measured.
- The Assessment of The Thorax and Lungs Including Lung Sounds: The size, symmetry, shape, and for the presence of any skin lesions and chest movements are observed. As well the breath sounds are observed and documented.
- The Assessment of The Cardiovascular System Including Heart Sounds: By listening to the heart sound it is observed that the heart is normal or not.
- The Assessment of The Head: The head movement is visualized over here.
- The Assessment of The Neck: The neck is visualized and the thyroid gland is inspected for any swelling and also for normal movement during swallowing.
- The Integumentary System Assessment: The color of the skin, the quality, distribution and condition of the bodily hair, the size, the location, color and type of any skin lesions are assessed and documented, the color of the nail beds, and the angle of curvature where the nails meet the skin of the fingers are also inspected.
- The Assessment of The Peripheral Vascular System: The peripheral veins are gently touched to determine the temperature of the skin, the presence of any tenderness, and swelling.
- The Assessment of The Breast and Axillae: The breasts are visualized to assess the size, shape, symmetry, color, and the presence of any dimpling, lesions, swelling, edema, visible lumps, and nipple retractions. The nipples are also assessed for the presence of any discharge, which is not normal for either gender except when the female is pregnant or lactating.
- The Assessment of The Abdomen: The abdomen is visualized to determine its size, contour, symmetry, and the presence of any lesions.
- The Assessment of The Musculoskeletal System: The major muscles of the body are inspected by the nurse to determine their size, and strength, and the presence of any tremors, contractures, muscular weakness and/or paralysis. All joints are measured for their full range of motion.
- The Assessment of The Neurological System: The Balance, gait, gross motor function, fine motor function and coordination, sensory functioning, temperature sensory functioning, kinesthetic sensations, and tactile sensory-motor functioning, as well as all of the cranial nerves, are measured.
- The Assessment of The Male and Female Genitalia and Inguinal Lymph Nodes: The skin and the pubic hair are inspected. The labia, clitoris, vagina and urethral opening are inspected among female clients. The penis, urethral meatus, and the scrotum are inspected among male clients.
- The Assessment of The Rectum and Anus: The rectum, anus and the surrounding area is examined for any abnormalities.
What Is a Comprehensive Health Assessment?
- Published On: January 3, 2020
A comprehensive health assessment gives nurses insight into a patient’s physical status through observation, the measurement of vital signs and self-reported symptoms. It includes a medical history, a general survey and a complete physical examination.
The general survey consists of a patient’s age, weight, height, build, posture, gait and hygiene. Nurses use health assessments to obtain baseline data about patients and to build a rapport with them that can ease anxiety and lead to a trusting relationship.
A comprehensive health assessment is generally conducted at the time of admission into an acute care facility or during the first visit to an outpatient clinic. When nurses perform an assessment, they may use techniques such as:
Inspection
This is the most frequently used method for assessment. Nurses look for indications of a health problem by using their eyes, ears and nose. They may inspect skin color, lesions, bruises or rashes as well as pay attention to abnormal sounds and odors.
Auscultation
Nurses listen to the sounds of the abdomen by placing the diaphragm or bell of a stethoscope on the bare skin of a patient.
Palpation
Nurses apply varying degrees of pressure on the patient with different parts of their hands. Palpation allows nurses to assess for texture, tenderness, temperature, moisture, pulsations and the presence of masses.
Percussion
Nurses firmly press on sections of a patient’s body with the distal part the middle finger on their non-dominant hand. The technique is used directly over suspected areas of tenderness to check a patient’s level of discomfort.
What Steps Are Involved in a Comprehensive Health Assessment?
Typically, a comprehensive assessment begins with documenting a patient’s health history before starting a physical exam. According to AMN Healthcare Education Services, the health history includes: the patient’s medical complaint, present state of health, past health record, current lifestyle, psychosocial status and family history.
The health history provides nurses with in-depth information about symptoms, childhood illnesses, related medical experiences and risks for developing certain diseases.
After the health history data is recorded, a physical is conducted which covers a review of the patient’s body systems. A head to toe examination includes assessments of the following:
- Skin
- Neurological function
- Ears, eyes, nose and throat
- Respiratory function
- Cardiac-pulmonary system
- Abdomen
- Muscles and joints
- Limbs, shoulders, hips, ankles and feet
- Reproductive system
- Nutrition
A thorough and accurate assessment is important because it helps differentiate the normal condition of the patient from the abnormal. And, a comprehensive health assessment establishes if a patient needs diagnostic testing or additional medical care.